
Real Event OCD - Signs and How to Recognize Them
Discover how Real Event OCD differs from typical OCD, focusing on real past or present events. Learn...
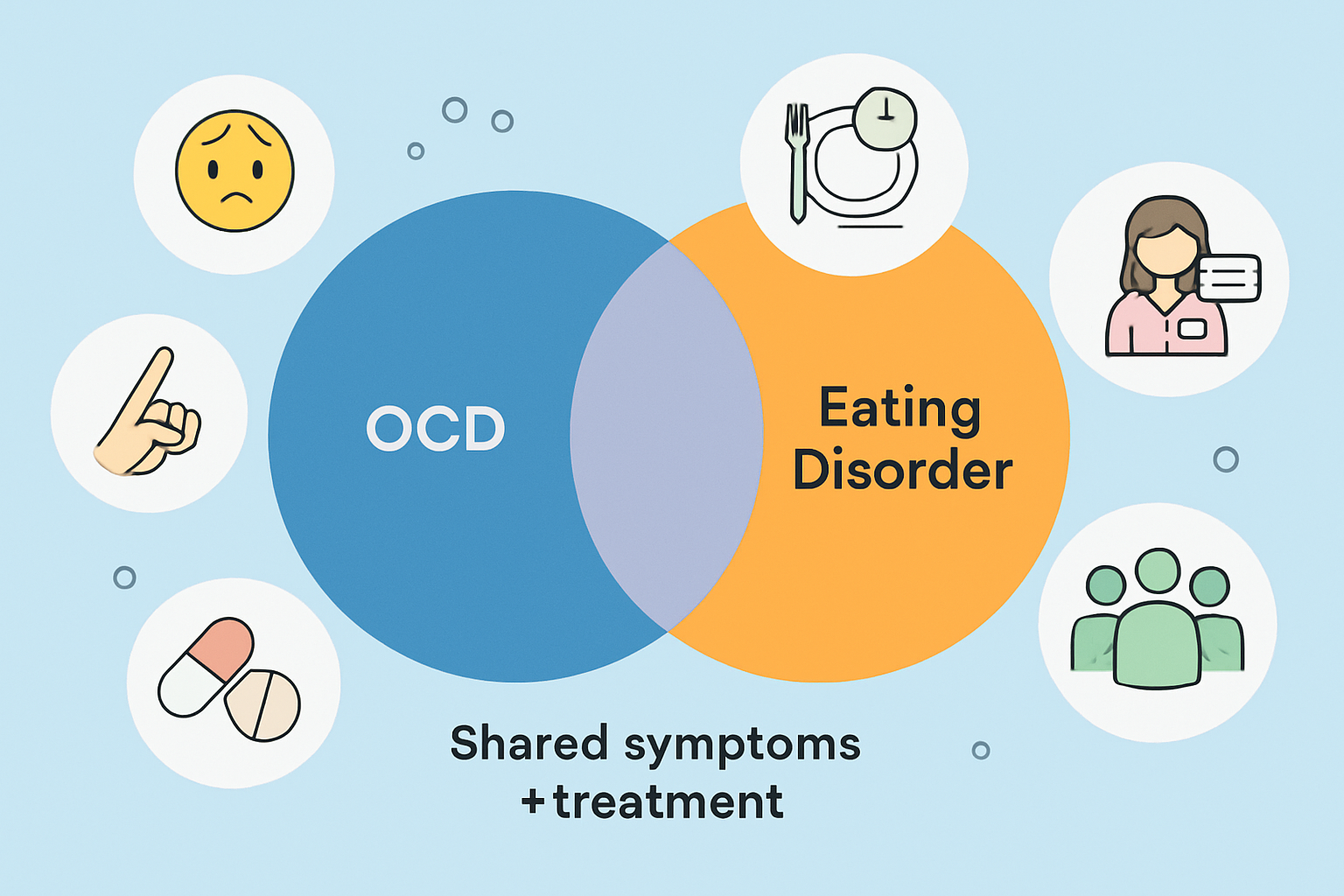
Obsessive-Compulsive Disorder (OCD) and eating disorders are distinct mental health conditions yet they often walk hand in hand. This creates a tricky tangle of challenges for those caught in both.
OCD is a condition that involves those pesky unwanted thoughts known as obsessions, paired with behaviors called compulsions that people perform to calm the anxiety these thoughts stir up.
Eating disorders are complex mental health conditions marked by unhealthy attitudes toward food and body image. The most common types—anorexia nervosa, bulimia nervosa and binge-eating disorder—involve severe and often harmful behaviors around food.
OCD and eating disorders share several symptoms such as repetitive behaviors and obsessive thoughts. This overlap can muddy the waters and make it tough to tell one from the other without a careful evaluation.
| Symptom/Behavior | OCD Characteristics | Eating Disorder Characteristics | Examples |
|---|---|---|---|
| Repetitive Behaviors | Compulsions carried out to ease that nagging anxiety | Ritualized eating habits or food-related routines done on repeat like clockwork | Washing hands over and over versus obsessively cutting food into tiny, almost hilarious, little pieces |
| Intrusive Thoughts | Unwanted, distressing thoughts (think contamination fears that just won’t quit) | Constant worries buzzing around body weight or shape | Fear of germs taking center stage compared to that persistent, sometimes exhausting, calorie counting |
| Anxiety Management | Performing rituals to calm the storm of anxiety | Tight control over eating habits to manage guilt or shame | Repeatedly double-checking the locks vs. skipping meals trying to grab some sense of control |
| Perfectionism | A strong need for everything to be just so, exactly right | Unrealistic body standards that push behaviors | Arranging objects with meticulous symmetry vs. chasing that flawless, often unreachable, body image |
| Avoidance | Dodging situations that can trigger those pesky obsessions | Steering clear of specific foods or social eating occasions | Side-stepping door handles compared to politely bowing out of eating in social settings |
| Control Issues | Feeling the urge to control thoughts or actions | Keeping a tight rein on food intake and body shape | Repeatedly checking tasks to feel in the driver’s seat vs. restricting food just to hold on to control |
OCD and eating disorders often have roots in similar places—think anxiety and perfectionism and the brain’s quirky way of handling stubborn intrusive thoughts and behaviors.
"My rituals started with food—counting every bite like it was some kind of secret code, and washing my hands as if my plate might be harboring a whole colony of germs. It was honestly tricky to untangle which thoughts belonged to OCD and which sprang from my anxiety about eating. But when I finally saw how they intertwined, it sparked a little hope for recovery, like a light at the end of a long, twisty tunnel."
OCD and eating disorders often sneak up due to a tangled web of overlapping risk factors. They arise from inherited genetic vulnerabilities and environmental stresses combined with psychological traits like anxiety and perfectionism.
Health professionals lean on thorough interviews and keen observations to tease apart OCD from eating disorders—especially when symptoms overlap and muddy the waters.
Managing both OCD and eating disorders often calls for a mix of strategies like cognitive-behavioral therapy, medication and nutritional guidance.
Treating both disorders simultaneously can be quite the juggling act since their symptoms often weave into one another in tricky ways. Tackling them together usually gives progress a nice little boost.
Supporting a loved one grappling with OCD and eating disorders can feel like walking a tightrope—tricky, but not impossible. It’s all about finding the right balance between patience and encouragement. A little empathy goes a long way, and sometimes just being there to listen (without jumping in with solutions) can mean the world. Remember, progress might be slow and full of bumps, but every small step forward is worth celebrating. Keeping an open mind and a light heart can help both of you navigate the ups and downs without losing sight of hope.
Helping someone wrestling with both OCD and eating disorders really demands a good dose of patience and genuine understanding. It’s important to avoid anything that might unintentionally feed into their compulsions or restrictive eating habits—trust me, those little triggers can sneak up on you.
It’s easy to mix these two up, but they’re not quite the same animal. While OCD often gets pegged for controlling thoughts and rituals, eating disorders have their own complex layers involving body image and food. People sometimes lump them together, but the reality is they dance to different rhythms, even when they might show up at the same party. Understanding the nuances helps us cut through the noise and really see what’s going on beneath the surface.
Many myths about OCD and eating disorders tend to muddy the waters when it comes to real understanding and genuine support. It’s so much more than just being a neat freak, and eating disorders are definitely not some kind of choice people casually make.

Discover how Real Event OCD differs from typical OCD, focusing on real past or present events. Learn...

Discover everything you need to know about OCD — from recognizing symptoms to effective treatments —...

Contempt is a toxic emotion that can erode love and respect in relationships. Discover what contempt...

Language processing disorder impacts how children understand and use language. Learn to recognize ea...