
Rumination Eating Disorder - Symptoms And Treatment
Rumination eating disorder involves repeated regurgitation of food without nausea. Understand its si...
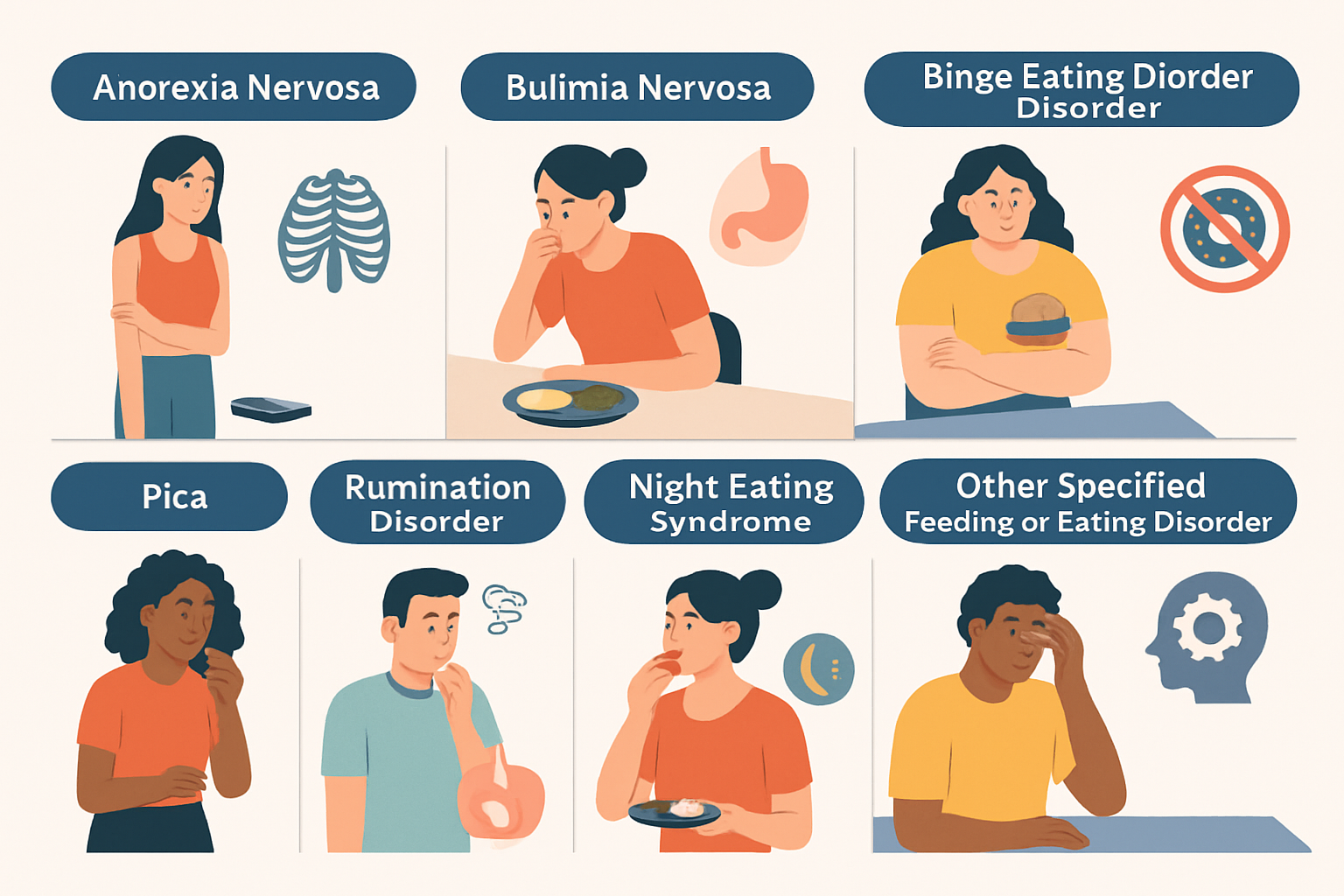
Eating disorders are complex mental health challenges that deeply impact physical and emotional well-being. Understanding the different types of eating disorders can make a difference in spotting them accurately, getting the right diagnosis and tailoring treatment to the individual.
Eating disorders cover a wide spectrum of unusual eating habits, from rigidly restricting food intake to those moments when bingeing feels absolutely out of control. These behaviors usually come tied to some form of psychological distress.
Eating disorders are serious mental health conditions that involve unusual or disrupted eating patterns and can take a real toll on both physical health and mental well-being. They usually arise from a mix of psychological, biological and environmental factors such as emotional stress, genetic predispositions and societal pressures. These disorders often reveal themselves through behaviors like restricting food intake, binge eating or avoiding certain foods altogether.
These disorders take a real toll on physical health and often lead to malnutrition, organ damage or a higher risk of death.
This guide dives into the eight eating disorders that tend to show up most often, each with unique behaviors and psychological roots. From well-known conditions like Anorexia Nervosa and Bulimia Nervosa to those you might not hear about as much like ARFID and Orthorexia, understanding what makes each one tick can foster empathy and sharpen diagnosis. It also helps tailor treatments that actually fit the person in front of you.
Let’s dive into the heart of the matter—grasping what anorexia nervosa truly involves. It’s not just about skipping meals or wanting to lose a few pounds; this condition runs much deeper, often entwining itself with emotions and perceptions in ways that can be hard to untangle. Understanding it fully means looking beyond the surface and acknowledging the complex web of mental and physical challenges it presents.
Anorexia Nervosa is about drastically cutting down food intake usually because of an intense fear of gaining weight and a skewed view of one’s own body. It often shows up in adolescent girls but can affect anyone regardless of gender or age. When doctors diagnose it, they look for alarmingly low body weight and behaviors that stop weight gain. They also look for psychological clues like denial about how serious the situation is.
There are two main subtypes to keep in mind. The first, known as the restricting type, is characterized by strict dieting and intense exercise routines—think of it as a relentless pursuit of control. The second is the binge-eating/purging type where episodes of overeating are followed by purging behaviors. This cycle can be difficult to break. Each subtype brings unique hurdles in treatment because patients often go to great lengths to hide their symptoms or resist putting on weight.
Getting a grip on what Bulimia Nervosa really is can feel like peeling back layers of a pretty complex onion. At its core, this eating disorder involves a vicious cycle of binge eating followed by some form of purging, whether it is vomiting, excessive exercise, or using laxatives. People often find themselves trapped in this exhausting loop, struggling to balance intense feelings around food and their body image. It’s not just about food—there's a tangled web of emotions and thoughts underneath, and understanding that is key to making any real progress.
Bulimia Nervosa is characterized by repeated episodes of binge eating followed by behaviors such as self-induced vomiting or laxative misuse or intense exercise to dodge weight gain. People dealing with this condition often maintain a normal or slightly higher than normal weight but wrestle with considerable psychological distress beneath the surface. Common symptoms include electrolyte imbalances, gastrointestinal troubles and dental erosion connected to purging.
Unlike anorexia, people with bulimia often see more ups and downs in their weight and usually keep a fairly clear sense of their body image. Still, they carry a heavy load of shame and guilt that can be really tough to shake. Diagnosing bulimia mostly comes down to how often these binge-purge episodes happen and how intense they get.
Binge Eating Disorder is characterized by repeated episodes where individuals consume large amounts of food in a short time without any purging. People often eat quickly and sometimes in secret. They are left feeling overwhelmed by guilt or disgust afterward. This disorder is closely tied to emotional battles like depression and anxiety. Unfortunately, it also brings a host of health issues such as obesity, diabetes and heart problems.
ARFID is marked by a selective palate often driven by sensory sensitivities or a genuine fear of choking. It can also stem from a complete lack of interest in eating without any worry about body weight or shape. It can lead to noticeable nutritional gaps and sometimes hampers growth, especially in kids and teens who need their nutrients. Unlike anorexia, where the focus is on controlling weight, ARFID is about steering clear of certain foods with no weight control involved.
Sometimes, not all eating disorders fit neatly into one box, and that’s where OSFED comes into play. It’s a bit of a catch-all category for those tricky cases that don’t hit every checklist item but still pack a punch in terms of impact. Think of it as the “other” folder on your desktop—easy to overlook, but containing stuff you really can’t ignore. People dealing with OSFED face serious challenges, and it’s important to recognize that even if it doesn’t look textbook, it’s just as real and deserving of attention and care.
OSFED covers eating disorders that cause a lot of distress or impairment but don’t quite check all the boxes for anorexia, bulimia or binge eating disorder. For instance, there’s atypical anorexia where someone’s weight might be in the normal range but their food intake is restricted. It also includes purging disorder and night eating syndrome.
Let's dive into the curious case of Pica, a condition that’s as puzzling as it sounds. Essentially, it’s the persistent craving and chewing of non-food items—think dirt, chalk, or even paper. Now, before you raise an eyebrow, this isn’t some quirky habit but a recognized medical condition with roots in nutritional deficiencies, mental health challenges, or sometimes just plain old stress. It’s more common in children and pregnant women, which makes you wonder what’s going on under the surface. Tackling Pica means more than just telling someone to stop—it’s about understanding the underlying causes and lending a hand with empathy and treatment. So, while it might seem odd at first glance, there’s often a lot more than meets the eye here.
Pica involves persistent munching on non-food items like dirt, paper or chalk for at least a month. This quirky habit is not just harmless nibbling because it can cause serious physical problems such as poisoning, intestinal blockages and infections.
Rumination Disorder involves the repeated act of bringing up food that might be re-chewed, swallowed again or spat out. It is almost like a quirky habit that won’t quit. Unlike vomiting, this behavior is voluntary and isn’t linked to gastrointestinal problems. You’ll often see it in infants, people with intellectual disabilities and sometimes adults under serious stress.
Orthorexia Nervosa hasn’t made its official debut in diagnostic manuals yet but is catching more attention in clinical circles. It is characterized by an intense obsession with eating only foods deemed pure or healthy. This can ironically lead to nutritional deficiencies and social isolation. What sets this condition apart is the focus on food quality rather than the quantity consumed or worries about body image—a different beast altogether.
Eating disorders come in all shapes and sizes with their own behaviors, psychological triggers, physical signs and ways to tackle treatment. Getting a handle on these differences is key
| Eating Disorder | Core Symptoms | Behavior Frequency | Typical Onset Age | Psychological Drivers | Health Risks |
|---|---|---|---|---|---|
| Anorexia Nervosa | Severely restricting food intake, coupled with a distorted body image | Avoiding food on a daily basis | Usually kicks in during adolescence | Overwhelming fear of gaining weight, paired with a streak of perfectionism | Malnutrition, with a scary risk of cardiac arrest |
| Bulimia Nervosa | Cycles of binge eating followed by purging, caught in a tough loop | Happening at least once a week | Most common in late teens to early twenties | Struggling with impulse control and carrying a heavy load of shame | Electrolyte imbalances, along with gastrointestinal damage |
| Binge Eating Disorder | Repeated bouts of binge eating without the purging phase | Frequent binge episodes, often hard to stop | Usually emerges in adulthood | Wrestling with emotional ups and downs, often tangled with guilt | Brings along health issues related to obesity |
| ARFID | Avoiding or restricting food without any worries about weight | Ongoing food avoidance, quite persistent | Most often noticed in childhood | Sensory sensitivities and a fear of unpleasant consequences | Malnutrition and growth problems |
| OSFED | Symptoms that don’t neatly fit into other major eating disorders | Highly variable | Can appear at any age | Causes differ depending on the specific subtype | Can be quite serious, depending on the case |
| Pica | Consuming non-food items, a puzzling behavior | Persistent and frequent | Often starts in childhood or during pregnancy | Nutritional gaps and complex mental health factors | Risk of toxicity and possible gastrointestinal blockage |
| Rumination Disorder | Repeatedly bringing back up and rechewing food | Happens often, sometimes daily | Can affect anyone from infancy through adulthood | Stress and developmental hurdles | Tends to cause esophageal damage and malnutrition |
| Orthorexia Nervosa | Obsessing over eating only what’s deemed 'pure' or 'healthy' | Compulsive daily habits | Typically begins in young adulthood | A need for control mixed with strong moral views about food | Nutritional shortfalls and social isolation can result |
Many symptoms often overlap such as food restriction or binge eating which can really muddy the waters when it comes to diagnosis.
Catching eating disorders early can truly be a game changer. Noticing subtle shifts in behavior or physical cues and emotional ups and downs often paves the way for faster intervention.
Families and friends are encouraged to respond to concerns with understanding and patience, creating a safe space for open conversations where judgment takes a backseat.
When it comes to tackling eating disorders, there’s no one-size-fits-all solution. The path to recovery often involves a mix of treatments tailored to individual needs—think of it as finding just the right recipe where every ingredient matters. From therapy sessions that help unpack the underlying issues to nutritional guidance that gets the body back on track, support systems play a huge role. And let’s not forget the power of community or peer groups, where sharing stories and experiences can feel like a lifeline. It’s a journey, sometimes winding and tough, but with the right help, things can and do get better.
Effective treatment for eating disorders usually involves a blend of psychological therapy, nutritional guidance and medical supervision. Sometimes medication is also involved.
Treatment plans need to be tailored to the specific disorder and its severity. The patient’s age and psychological factors are also important. Early intervention often leads to better outcomes, but recovery is usually a marathon not a sprint.
"Taking an integrated approach that looks at the physical, psychological, and social aspects of eating disorders usually turns out to be the secret sauce for truly lasting recovery. And, from what I’ve seen, ongoing support after the initial therapy can really make all the difference—helping individuals rebuild their health while also boosting their resilience in ways that stick." – Dr. Sarah Mitchell, Clinical Psychologist specializing in Eating Disorders
Prevention focuses on encouraging balanced eating habits and nurturing a healthy body image, especially when dealing with different types of eating disorders. It also fosters resilience when confronting societal pressures that can sometimes feel overwhelming.
Keep an eye out for changes like avoiding food or eating in secret and becoming overly obsessed with body image. Physical signs might appear such as sudden weight swings or dizziness and stomach issues that won’t quit. Emotional challenges like pulling away from friends or family or exercising beyond healthy limits can also raise red flags. It’s important to approach them gently and suggest seeing a professional—kindness goes a long way with this delicate topic.
Orthorexia Nervosa hasn’t made it into official manuals like the DSM-5 yet but more clinicians are recognizing it these days. It’s an unhealthy fixation on eating only ‘clean’ or ‘pure’ foods that can lead to nutritional gaps and social isolation. Treatment often involves loosening rigid food rules and tackling the anxiety underneath.
ARFID is very different from being a picky eater. It involves intense food avoidance due to sensory sensitivities, fear of choking, or lack of interest in eating. This often causes malnutrition or stunted growth. Unlike picky eaters, people with ARFID restrict their diets so much it seriously impacts their health. That’s when professional help usually becomes necessary.
Eating disorders often start in adolescence but can develop at any age, even adulthood. Stress in midlife, hormonal changes, or trauma can trigger disordered eating. Older adults face challenges like misdiagnosis since symptoms overlap with other health issues. It’s key to keep an open mind about eating disorders across all ages.
The best first move is to reach out to a healthcare provider or mental health professional for an evaluation. Early intervention makes a big difference and these experts can guide you to the right treatment, whether therapy, nutritional counseling, or medical care. Don’t underestimate the power of talking with a trusted friend or family member for support.
Yes, medications like antidepressants—SSRIs in particular—can help manage anxiety or depression that often come with disorders like Bulimia Nervosa or Binge Eating Disorder. However, they are generally part of a bigger treatment plan that includes therapy and nutritional support. No pill alone can do the heavy lifting with eating disorders.

Rumination eating disorder involves repeated regurgitation of food without nausea. Understand its si...

Pica disorder involves the persistent eating of non-food substances. Learn what causes this conditio...

Anorexia nervosa often evokes images of extreme thinness, but can you be overweight and anorexic? Th...

Contempt is a toxic emotion that can erode love and respect in relationships. Discover what contempt...