
Quiet Borderline Personality Disorder - Symptoms to Recognize
Quiet borderline personality disorder is a hidden form of BPD marked by intense internal struggles....
Schizophrenia and Multiple Personality Disorder are often confused although they’re two distinct mental health conditions with their own symptoms, causes and treatment approaches.
Schizophrenia is a long-term mental health condition that deeply impacts a person’s thoughts and feelings. It typically kicks in during late adolescence or early adulthood and can throw a wrench in how someone perceives reality and handles their emotions.
The exact cause of schizophrenia isn’t completely nailed down but it appears to stem from a mix of genetic, biological and environmental factors all playing their part. If you have a family history your odds might be a bit higher and imbalances in brain chemicals like dopamine often stir the pot.
Multiple Personality Disorder, now called Dissociative Identity Disorder (DID), is having two or more distinct identities or personality states inside a single person. Each identity usually has its own name and backstory.
DID usually crops up as a psychological shield when someone goes through severe trauma, especially repeated abuse or neglect in childhood. The brain crafts separate identities to tuck away those tough memories and feelings. This makes it easier for the person to get through the day. Trauma is definitely a big piece of the puzzle.

| Aspect | Schizophrenia | Dissociative Identity Disorder (DID) |
|---|---|---|
| Definition | A psychotic disorder where reality gets a bit warped, leading to altered perceptions | A dissociative disorder in which a person has multiple distinct identities, sometimes quite noticeably |
| Main Symptoms | Hallucinations, delusions, and thinking that can be pretty confusing at times | Memory lapses, sudden switches between identities, and episodes where reality feels fragmented |
| Causes | A complex cocktail of genetic factors, brain chemistry, and environmental influences | Severe trauma, often rooted in childhood abuse, that leaves lasting marks |
| Typical Onset Age | Usually pops up in the late teens to early adulthood | Often diagnosed during adulthood, though the trauma usually dates back to early life |
| Diagnostic Criteria | Psychotic symptoms that stick around for at least six months (according to DSM-5) | Presence of at least two distinct identities, along with noticeable memory gaps |
| Treatment Approaches | A combination of antipsychotic meds, therapy, and rehab efforts | Therapy focused on trauma healing, symptom-targeting medications, and supportive care |
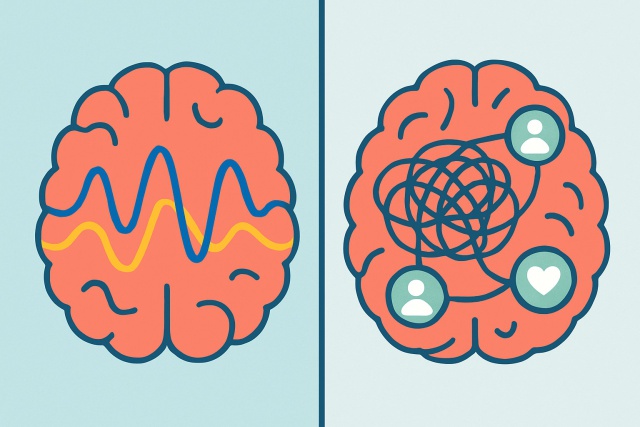
Schizophrenia and DID often get tangled up in people’s minds largely thanks to how they’re portrayed in movies and TV shows. But in reality, they’re quite different beasts. Schizophrenia primarily messes with how someone experiences the world and processes their thoughts, whereas DID revolves around a break in identity that usually stems from trauma.
Diagnosing schizophrenia and DID usually starts with thorough clinical interviews and psychological evaluations—no shortcuts here. Mental health pros really zero in on symptom patterns and patient history, leaning on established diagnostic guidelines to pin down the right condition.
Treatment for schizophrenia often relies on antipsychotic medications to reduce hallucinations and delusions. Psychotherapy especially cognitive behavioral therapy (CBT) plays a key role in managing symptoms and helping people develop stronger coping strategies. Psychosocial rehabilitation helps rebuild social skills and daily functioning.
When it comes to DID, psychotherapy—especially trauma-focused therapy—really takes center stage for helping to weave together those separate identities and gently unpack those tough traumatic memories. Medications can come into play too, mainly to tackle symptoms like depression or anxiety that often tag along.
Individuals living with schizophrenia often struggle with social isolation, holding onto jobs and managing symptoms that twist their sense of reality. Those with DID face hurdles like identity confusion and memory gaps that can deeply impact their relationships and daily life.
Understanding the differences between schizophrenia vs multiple personality disorder is crucial, as having a solid support system from family, friends and mental health professionals makes a world of difference when managing either condition. Approaches such as therapy, staying on top of prescribed medications and keeping a structured routine usually help improve stability and boost overall quality of life.
"Showing a bit of understanding and genuine compassion goes hand in hand with clinical treatment when we are helping individuals with schizophrenia and DID live meaningful lives. Raising awareness isn’t just a nice idea—it’s key to busting stigma and laying down the groundwork for real recovery and ongoing support."

Quiet borderline personality disorder is a hidden form of BPD marked by intense internal struggles....

Discover rare mental disorders that affect few but have profound impacts, covering symptoms, diagnos...

Schizoaffective disorder combines symptoms of schizophrenia and mood disorders, often causing confus...
Confused about bipolar disorder versus borderline personality disorder? This guide breaks down their...