
Reactive Attachment Disorder in Adults - Signs and Symptoms
Reactive Attachment Disorder in adults often goes unrecognized. Learn about its key symptoms, causes...
Rare mental disorders are a cluster of psychiatric conditions that fly under the radar for most people, including quite a few healthcare professionals.
Mental health spans a broad spectrum, ranging from everyday struggles like depression to rare conditions with a tangle of complex symptoms. Some of these disorders are pretty uncommon, research and awareness often fly under the radar.
Rare mental disorders are psychiatric conditions that affect a tiny fraction of the population—usually pegged by international standards at fewer than 1 in 2,000 people. Diagnosing them can be quite the challenge since their symptoms tend to mimic those of more common disorders, making it tricky to pinpoint.
Limited awareness among both the public and professionals often results in poorer health outcomes and less research funding. Unfortunately, it also causes greater stigma—factors that seriously hinder access to effective care for those affected.
People living with rare mental disorders often find themselves up against a double whammy: juggling their symptoms while navigating a healthcare system that, frankly, isn’t always tuned in to their unique challenges. Raising awareness is not just a nice-to-have; it’s absolutely essential if we want to move the needle in a meaningful way. - Dr. Maria Henderson, Psychiatrist specializing in rare neuropsychiatric conditions
This guide dives into a handful of rare mental disorders picked for their unusual symptoms and notable clinical significance. It also covers the diverse challenges they present.
Capgras Syndrome is one of those rare and puzzling conditions where people become absolutely convinced that their close friends or family members have been swapped out for impostors. It involves symptoms of misidentification and usually shows up alongside neurological damage or psychotic disorders.
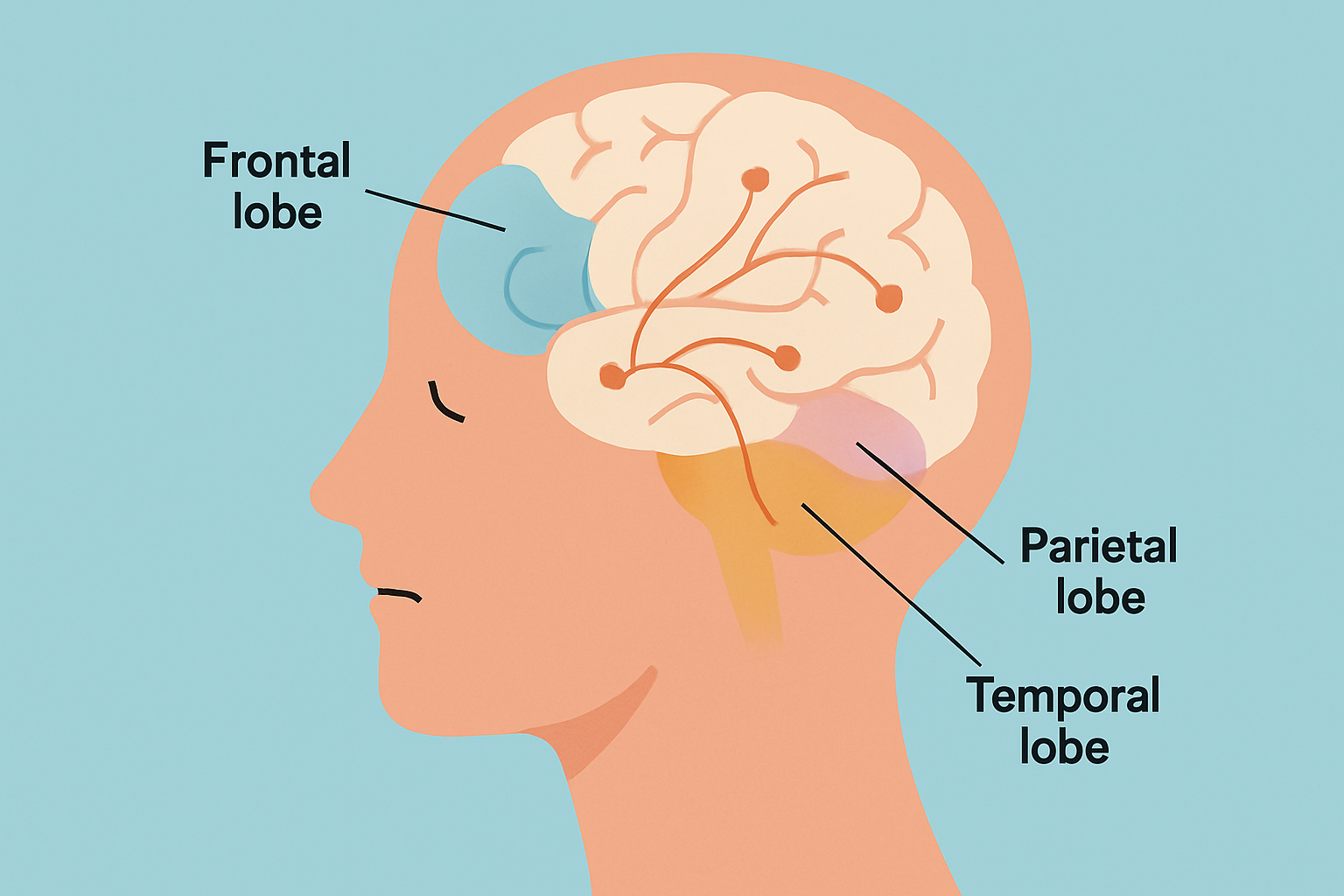
Cotard's Delusion, sometimes called Walking Corpse Syndrome, is a truly unsettling condition where people become convinced they don’t exist or that parts of their body have vanished. It usually springs from neurological glitches involving the parietal lobes or their connections to emotional centers in the brain. Those living with this disorder often wrestle with severe depression and bizarre delusions about being immortal or already dead. They also tend to neglect their own care. Treatment usually involves antidepressants, antipsychotics and sometimes electroconvulsive therapy (ECT).
Alice in Wonderland Syndrome brings about fleeting perceptual quirks where people might suddenly feel like their body parts or nearby objects have played a trick on their eyes and appear oddly sized or shaped. It is often linked with migraines, epilepsy or viral infections and usually shows up in children. When it comes to treatment the goal is to track down those pesky triggers and ease the symptoms.
Ever met someone you were convinced was playing hide-and-seek with your identity? That’s the curious case of Fregoli Delusion—a quirky but unsettling condition where a person believes different strangers are actually the same individual in disguise. It’s like their mind insists on a one-person show, no matter how many actors take the stage. This delusion can really throw a wrench in social interactions, turning everyday encounters into a maze of suspicion and confusion. In my experience, understanding this peculiar twist of perception can feel like trying to untangle headphones in the dark—tricky, but deeply fascinating.
Fregoli Delusion is a rare psychiatric disorder where people become convinced that different individuals they see are actually one person in disguise with various appearances. This often comes with feeling persecuted and can make life challenging. It is thought to be connected to brain lesions in the right hemisphere, adding a neurological twist. Treatment usually involves antipsychotic medications and cognitive-behavioral therapy.
Kleine-Levin Syndrome is characterized by recurrent episodes where a person crashes into prolonged sleep lasting days or sometimes weeks. Alongside these marathon naps, people often experience foggy thinking and confusion. Noticeable shifts in behavior include suddenly eating way more than usual or showing an increased sexual drive. The root cause remains a bit of a mystery but is generally thought to involve hiccups in the hypothalamus. Treatment mainly revolves around symptom management and support.
Symptoms seen in rare mental disorders often show up as changes in identity, unusual perceptions or sudden deep mood swings. Shifts in thinking might leave you scratching your head. These signs can easily overlap with those from more common conditions.
| Disorder | Core Symptoms | Typical Misdiagnoses | Diagnostic Techniques | Available Tests |
|---|---|---|---|---|
| Capgras Syndrome | A strange and unsettling belief that people you know well have been swapped out for impostors | Often mistaken for Schizophrenia or Dementia | Careful clinical interviews paired with neuroimaging usually do the trick | MRI scans and neuropsychological assessments are commonly used |
| Cotard’s Delusion | Deeply nihilistic delusions around death or the sense that one simply does not exist | Frequently confused with Severe depression or Psychosis | Thorough psychiatric evaluation alongside EEG monitoring is key | Neurological imaging helps shed light here |
| Alice in Wonderland | Bizarre distortions in how size and visuals are perceived, as if reality itself is playing tricks | Often misdiagnosed as Migraine aura or Epilepsy | Diving into patient history and EEG tests usually reveals the truth | MRI scans and EEG recordings come in handy |
| Fregoli Delusion | The odd conviction that different people are actually one single person in clever disguise | Commonly confused with Paranoid schizophrenia | Clinical observation combined with brain imaging tends to clarify things | CT scans and MRI scans are standard fare |
| Kleine-Levin Syndrome | Recurrent episodes of sleeping way too much, coupled with noticeable shifts in cognition and behavior | Can be mistaken for Narcolepsy or Depression | Detailed sleep studies paired with neurological assessments are essential | Polysomnography is the go-to test |
Treatment for rare mental disorders usually calls for a blend of medication and therapy plus newer tricks like neuromodulation. All are wrapped up in a coordinated care plan tailored to each person’s unique symptoms and needs.
One major challenge in providing effective treatment is the limited number of clinical trials, often due to small patient populations and a shortage of specialized providers.
People living with rare mental disorders often wrestle with feelings of isolation and being misunderstood and the frustration of uneven access to care.
"For the longest time, I felt pretty invisible, like my struggles flew under the radar because my condition is so rare. Then, stumbling upon others who truly understand what it’s like flipped the script and seriously lightened the load of managing my disorder." – Eliot, living with Capgras Syndrome
Sometimes, finding the right help feels like searching for a needle in a haystack, but luckily, there are plenty of resources and support networks out there ready to lend a hand. Whether you’re looking for advice, guidance, or just someone who gets where you’re coming from, these connections can make all the difference. Think of them as your trusty sidekicks on this journey—always nearby and ready when you need a boost.
Current research often zeroes in on pinpointing biological markers and improving diagnosis with neuroimaging. It also crafts personalized medicine approaches tailored to individual needs.
Advances in technology and data science are quietly reshaping how rare mental disorders get diagnosed and treated. Machine learning algorithms can dig through complex neuroimaging and genetic data to uncover subtle patterns that often slip past even the sharpest clinicians. Digital health platforms make it easier to keep tabs on symptoms and patient-reported outcomes and help deliver care that’s not just timely but spot-on. Telepsychiatry opens doors to specialists who might otherwise be out of reach because of distance or scarce resources.

Reactive Attachment Disorder in adults often goes unrecognized. Learn about its key symptoms, causes...

Quiet borderline personality disorder is a hidden form of BPD marked by intense internal struggles....

Learn to differentiate Narcissistic Personality Disorder from Borderline Personality Disorder by und...
Confused about bipolar disorder versus borderline personality disorder? This guide breaks down their...